Living with Retinal Vein Occlusion: Causes, Symptoms, and Treatment Options
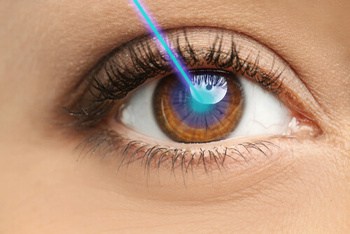
Imagine waking up one morning to find your vision blurred or distorted in one eye. You may have just experienced the onset of retinal vein occlusion, a condition that affects the blood vessels in the retina and can lead to vision loss. In this comprehensive guide, we will discuss the causes, symptoms, and treatment options for both central and branch retinal vein occlusion, as well as how to adapt to life living with retinal vein occlusion and maintain an optimal quality of life.
Understanding Retinal Vein Occlusion
Retinal vein occlusion is a condition estimated to affect one to two per cent of those over 40, the majority being aged 60 and above. It occurs when veins in the retina become obstructed by blood clots – leading to vision loss, retinal swelling/haemorrhage and damage caused directly due to cell disruption. There are two types:
Central Retinal Vein Occlusion (CRVO) affects larger veins and results in more severe forms of sight impairment.
Branch Retinal Vein Occlusions (BRVOs) occur as blockages within smaller branches, causing less serious effects on vision overall.
These conditions target only Veins, unlike similar issues that can involve arterial disruptions – such as a central retinal artery or an afflicted branch-off thereof, thereby differentiating it from other physical problems affecting parts around the eyes relatedly but not exclusively with regards to ailments pertinent solely towards retinal vessels specifically.
Central Retinal Vein Occlusion (CRVO)
Central Retinal Vein Occlusion (CRVO), commonly known as Retinal Vein Occlusion, is a serious eye condition that occurs when the primary drainage pathway of blood from the retina becomes blocked. Risk factors for developing CRVO are high blood pressure, hyperlipidemia, smoking and diabetic retinopathy.
At the same time, its complications can include Macular Oedema due to leakage or growth in abnormal new Blood Vessels, leading to elevated Intraocular Pressure with potential pain and vision loss, worsening prognosis. Ischemic and Non-ischemic types have their own characteristics resulting from central Retina Venous blockage causing direct impairment of one’s sight if not correctly treated promptly.
Branch Retinal Vein Occlusion (BRVO)
Branch retinal vein occlusion (BRVO), caused by the blockage of a smaller retinal vein, affects between 0.64% and 2.74% of individuals worldwide. Possible causes include age-related factors, hypertension, diabetic retinopathy as well as atherosclerosis and smoking habits being risk factors for BRVO’s occurrence. Symptoms may range from loss or blurred vision in some parts to painless total sight decrease with floaters. Eye aches can also be included amongst those affected by this condition, while it can manifest through gradual or sudden deterioration in visual ability, too.
The main reason behind impaired eyesight that is linked with branch Retina Vein Occlusions would have to do with Macular Oedema, an accumulation of fluid around the macula due to obstruction on branches operating within the retina, leading to problems when processing sharp, detailed pictures correctly, which will then result in cloudy/ distorted visions eventually impairing overall visibility noticeably if not treated properly soon enough.
Risk Factors and Causes
Retinal vein occlusion has several risk factors, including high blood pressure, elevated intraocular pressure, diabetes retinopathy and high cholesterol. Some of these are modifiable with lifestyle changes that can lower the chances of this occurring or reduce its severity, such as controlling one’s blood sugar levels if diabetic, cessation of smoking activities and managing both high blood pressure and LDL-Cholesterol Levels effectively. Diagnosis is possible from an optometrist who may refer you to an ophthalmologist for treatment management strategy concerning all aspects of its initial cause factor(s).
Recognising Symptoms
Early detection and treatment of retinal vein occlusion are essential for successfully managing the complications that come with it. Blurry vision or sudden decline in visual acuity might be warning signs to look out for, as well as distorted sight and discomfort.
Even if the dominant eye adapts so one does not see a difference when focusing on their impaired eye, prompt medical attention is still needed to ensure proper prognosis can be achieved through effective care. Retinal vein blockage should not be overlooked since even minor symptoms such as fallouts may lead to serious issues related to eyesight overall.
Diagnosis Process
When diagnosing retinal vein occlusions, optometrists usually perform eye tests and ask questions about medical history. Diagnostic imaging may include Optical Coherence Tomography (OCT) to obtain cross-sectional images of the retina, which can reveal alterations in macular capillaries or a decrease in non-perfusion area.
This is supplemented by a fluorescein angiogram – an additional examination assessing blood vessels within the same region. Doctors might also take measurements of cholesterol levels, sugar and blood pressure readings as part of their overall assessment process for optimum health.
Treatment Options for Retinal Vein Occlusion
Treatment options for retinal vein occlusion include anti-VEGF injections, medications to manage the risk factors and laser treatment. Anti-VEGF injections inhibit the growth of abnormal blood vessels behind the eye, which can lead to macular oedema, while intravitreal injections deliver medication directly into a fluid in the eyeball to treat such swelling or new vessel formation.
Laser therapy is also used to close leaking vessels and reduce retina oedema, whereas retinal vein cannulation involves introducing a small tube that helps restore normal blood flow back through affected veins should all other treatments be ineffective. Steroid shots may occasionally be given when vascular endothelial growth factor (VEGF) inhibitors are deemed inadequate, as well as utilising lasers alongside drugs to help bring down inflammation & haemorrhaging associated with this condition.
While it is not possible to completely reverse vision loss caused by RVO, treatment aims at slowing future deterioration along with preventing any more severe damage via regular follow-up appointments where potential signs from newly developed dangerous blood vessels must continually be monitored and managed accordingly.
Adapting to Life with Retinal Vein Occlusion
Living with retinal vein occlusion necessitates lifestyle changes, as well as the utilisation of both low-tech and modern technology. Accessing emotional support systems is also essential in order to manage living with this type of vision loss effectively.
Low-tech resources such as large print materials, magnifying glasses, and telephones adapted for enlarged numbers are especially beneficial for those who suffer from retinal vein occlusion daily activities. Smartphone applications tailored towards people struggling with low vision can provide a sense of autonomy, which will help them remain independent when participating in everyday life events.
For individuals affected by these conditions, obtaining guidance through family members or mental health professionals, plus taking part in support groups, may aid greatly while managing feelings associated with their condition. Being equipped mentally equips one better emotionally since it has an impact on overall well-being, too. Retinal vein problems come accompanied by physical and psychological concerns that should be taken into account just like any other factor related to eye care issues due to its wide-ranging repercussions over the quality of life.
Lifestyle Changes and Prevention
When it comes to retinal vein occlusion, safeguarding yourself from risk factors by leading a healthy lifestyle and following prescribed treatments is imperative. Research has shown that exercising can be beneficial in reducing the occurrence of this condition.
Regular physical activity helps:
- Enhance cardiovascular health, which lowers potential blockages in veins – such as those at the back of your eyes;
- Keep body weight within recommended limits and
- Manage blood pressure levels optimally.
Consequently, all these elements are essential for avoiding retinal vein occlusion problems in general. Medications may also be administered when needed to control risk factors like high blood pressure, diabetes or cholesterol while minimising clot formation – one more factor associated with this vascular issue regarding vessels located at the retina’s edge specifically.
Emotional and Psychological Support
For individuals diagnosed with retinal vein occlusion (RVO), securing emotional and psychological support is of paramount importance. This support can be garnered from a range of sources, such as close family, mental health specialists, or dedicated support groups. Through the compassion, informed understanding, and assistance provided by these pillars of support, individuals with RVO can more effectively navigate their well-being. Additionally, therapeutic and counselling sessions can offer valuable tools to address the challenges associated with this condition.
Joining a specific kind of group that provides understanding among participants who are living similar experiences might be very beneficial in exchange for information for coping strategies, which could prove highly advantageous regarding managing the physical ailment’s effects psychologically. Accessing such aid would likely reduce any negative emotions associated with having retinal vein occlusion issues, so even if no one else understands how someone feels, they will have another outlet where recognition exists genuinely.
Driving with Retinal Vein Occlusion
For those with retinal vein occlusion, maintaining good vision in the unaffected eye is of utmost importance for driving safely and legally. Different jurisdictions have different minimal visual acuity needs for drivers suffering from this condition. Adequate sight must be present to drive even if regulation requirements are met.
To assist individuals facing retina-related challenges when it comes to operating a vehicle securely – steps can be taken such as installing wider side mirrors or rearview cameras, which will expand visibility range along with ensuring that dashboard lighting and controls are lit up properly during nighttime use, etcetera.
Tinted windows plus sunshades also come into play here, together with alterations on one’s seat configuration/positioning relative to their steering wheel, all of which should reduce strain while helping them navigate staircases & exercise machines better and handle hot liquids more confidently, too, since depth perception could potentially become an issue due to condition mentioned above known as retinal vein occlusion so regular pauses ought also to take place throughout longer journeys accordingly).
Prognosis and Recovery
 When it comes to retinal vein occlusion, the prognosis can differ depending on its severity. About a third of people recover without intervention. For another third, there is no change in condition. While remaining patients experience vision decline. Though symptoms are mild, many may manage full restoration with proper care. On the contrary, however, those inflicted by severe types tend to suffer irreversible damage, often leading to diminished sight – only a 50-60% chance of recovery exists here despite any treatment attempted.
When it comes to retinal vein occlusion, the prognosis can differ depending on its severity. About a third of people recover without intervention. For another third, there is no change in condition. While remaining patients experience vision decline. Though symptoms are mild, many may manage full restoration with proper care. On the contrary, however, those inflicted by severe types tend to suffer irreversible damage, often leading to diminished sight – only a 50-60% chance of recovery exists here despite any treatment attempted.
Many aspects play into how an individual’s case will progress, such as the type and intensity of initial affliction. Presence (or lack) of risk factors, including age and overall health state; management system that considers all associated risks present. The duration also varies among sufferers, given differences exist concerning their physical/ocular status plus response towards therapy provided if applicable.
Prognoses tied up with retinal vein occlusions vary greatly depending upon the situation per se – some do get better. In contrast, others might not have much luck despite efforts made, thereby underlining the importance of timely diagnosis & properly tailored interventions pertinent to that!
Coping with Vision Loss
People coping with retinal vein occlusion-caused vision loss should seek emotional and professional support to ensure optimal quality of life. Adjustments to daily activities are recommended, along with exploring rehabilitation programs and assistive technology options for low vision conditions due to this medical issue. Vision rehab supplies strategies and tools to make the most out of existing sight abilities. These techniques may help improve functioning as well as enhance independence in everyday living tasks.
Examples include magnifying glasses or devices such as oversized phones, large print materials or apps designed specifically for those affected by regional blindness status. By taking advantage of both high-tech solutions and simple equipment like magnifiers, one can maintain a good lifestyle while dealing with diminished eyesight resulting from their condition.
Frequently Asked Questions
How can I improve my retinal vein occlusion?
Treating a retinal vein occlusion may involve anti-VEGF injections, steroid injections and laser treatment or panretinal photocoagulation (PRP). All these therapies can help reduce macular edema associated with this kind of occlusion. They could prevent it from developing further.
Can you drive with retinal vein occlusion?
Provided the vision in your undamaged eye meets the DVLA’s set standards, driving is permissible when you have retinal vein occlusion.
What distinguishes Central Retinal Vein Occlusion (CRVO) from Branch Retinal Vein Occlusion (BRVO)?
Central Retinal Vein Occlusion (CRVO) occurs when there’s an obstruction in the primary retinal veins, leading to a more profound visual impairment compared to Branch Retinal Vein Occlusion (BRVO), which arises due to the blockage in one of the smaller branch veins. The extent of vision loss with BRVO is typically less severe owing to its localised nature.
 Is pain a manifestation of retinal vein occlusion?
Is pain a manifestation of retinal vein occlusion?
Indeed, retinal vein occlusion can manifest as ocular discomfort or pain. The root cause of this discomfort is the hindered circulation resulting from a blocked retinal vein. This obstruction subsequently triggers swelling and inflammation within the eye. If left unchecked, the progressing inflammation can exacerbate the discomfort and pain levels.
What symptomatic indications should one watch for in retinal vein occlusion?
Individuals with retinal vein occlusion might observe a sudden blur or diminished vision in a segment or the entirety of one eye. They may also perceive floating specks or web-like structures and might experience discomfort or pain in the eye involved.
How is retinal vein occlusion diagnosed?
A diagnosis of retinal vein occlusion is usually made through a comprehensive eye examination. This can include visual acuity testing, a dilated eye exam, and imaging tests like fluorescein angiography and optical coherence tomography.
Are there any lifestyle changes I can make to prevent retinal vein occlusion?
Yes, maintaining a healthy lifestyle can help prevent retinal vein occlusion. This includes regular exercise, a balanced diet, maintaining a healthy weight, and avoiding smoking. It’s also important to manage any underlying conditions like diabetes, high blood pressure, and high cholesterol.
Is retinal vein occlusion a permanent condition?
The extent of vision loss and the potential for recovery vary widely with retinal vein occlusion. Some people may regain much of their lost vision, while others may not see any improvement. Regular follow-ups with your ophthalmologist are crucial for managing this condition.
Summary
Retinal vein occlusion can lead to vision loss, so it is important for those living with the condition to recognise its causes, symptoms and treatment options. Taking necessary steps such as making lifestyle changes and utilising assistive technology may help maintain quality of life. Managing risk factors like high blood pressure or diabetes might also reduce one’s chances of suffering from retinal vein occlusion-related vision impairment. Psychological support can be beneficial in coping effectively with this condition, too.
Note: Any surgical or invasive procedure carries risks. Before proceeding, you should seek a second opinion from an appropriately qualified health practitioner.
Sources
Nick Astbury, FRCP Clinical Associate Professor, “Living with retinal eye occlusion” Guide Dogs. Jul 28, 2022
https://www.guidedogs.org.uk/getting-support/information-and-advice/eye-conditions/retinal-vein-occlusion/living-with-retinal-vein-occlusion/
Liao, Sharon, “What is retinal vein occlusion” WebMD. Sep 1, 2023
https://www.webmd.com/eye-health/retinal-vein-occlusion
G Atma Vemulakonda, MD, “What Is Branch Retinal Vein Occlusion (BRVO)?” American Academy of Ophthalmology. Oct 16, 2023
https://www.aao.org/eye-health/diseases/what-is-branch-retinal-vein-occlusion
“Central Retinal Vein Occlusion (CRVO)” National Eye Institute. Jul 09, 2022
https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/central-retinal-vein-occlusion-crvo
“Retinal Vein Occlusion (RVO)” Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/14206-retinal-vein-occlusion-rvo






Leave a Reply
Want to join the discussion?Feel free to contribute!